
Findings from a survey of college students examining beliefs about UV exposure and sunscreen use and their associations with skin cancer risk and UV protective behaviors provide some insights for patient counseling.

Findings from a survey of college students examining beliefs about UV exposure and sunscreen use and their associations with skin cancer risk and UV protective behaviors provide some insights for patient counseling.

Findings of initial studies and call for further testing should not be misconstrued to mean ingredients are unsafe.
Treatment for Merkel cell carcinoma has evolved due to the high aggressiveness and metastatic rate of the tumors. Immune checkpoint inhibitor therapy may change prognosis and quality of life.

The biology of nonmelanoma skin cancers and their strong immunogenicity makes these tumors good candidates for novel and emerging immunotherapeutic agents.

The U.S. Food and Drug Administration has approved pembrolizumab for cutaneous squamous cell carcinoma whose disease has shown to not be curable by radiation or surgery.

In case you missed it, this week we featured stories involving blastic plasmacytoid dendritic cell neoplasm (BPDCN), development of a biosimilar to BOTOX, a new nonmelanoma treatment device, the latest phase 3 results for abrocitinib in atopic dermatitis, results from a long-term dabrafenib and trametinib study in stage 3 BRAF-mutated melanoma, plus many more.

A new systemic medication option offers promising results for patients with high-risk squamous cell carcinoma for whom surgery has not worked, says this expert.
Fruits and vegetables rich in vitamin A appear to play a significant role in helping to decrease the incidental risk of developing squamous cell carcinoma, according to a recent study.

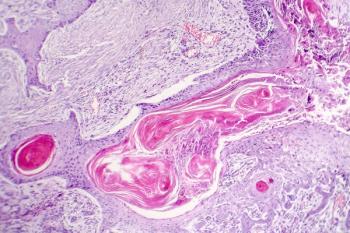
New German basal cell carcinoma (BCC) guidelines are more alike than unlike U.S. guidelines, although minor differences exist in areas such as prevention and newer systemic treatments, says experts.

Researchers recently examined a non-invasive test that, if additional studies can confirm, may directly affect future patient care for patients at risk for non-melanoma skin cancer.

Combined imaging modalities may help guide choice of treatment and prevent biopsy, according to one expert.

Read about the recent advancements in noninvasive imaging modalities that are making an impact on dermatological care.

In this pipeline report, Dermatology Times presents insights into Hh pathway inhibitors currently in phase 2 and phase 3 for the treatment of basal cell carcinoma.
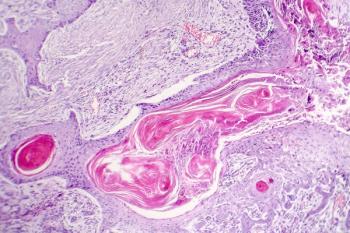
Better awareness in disease progression and improved understanding of field cancerization has shifted the thinking in management of patients with squamous cell carcinoma.

Are your patients are looking for alternatives to surgery for non-melanoma skin cancer? Superficial radiation therapy (SRT) may be the answer.

Superficial radiation therapy is experiencing a renaissance in dermatologic therapy due to the modernized equipment and updated guidelines, as well as excellent treatment outcomes for patients with NMSC which rival those seen with other approaches, including Mohs surgery.

The FDA has approved STP705, an siRNA (small interfering RNA) therapeutic for in situ Squamous Cell Carcinoma Nonmelanoma Skin Cancer (NMSC), to proceed with phase two clinical trials.
The past decade has seen significant advances in the understanding of molecular pathogenesis of skin cancer leading to the development of targeted treatments and immunotherapies that have dramatically improved progression free survival and even overall survival in melanoma, basal cell carcinoma (BCC) and even some rarer cutaneous carcinomas.

Topical 5‐fluorouracil is FDA-approved to treat actinic keratoses and superficial basal cell carcinoma, but it is commonly used off-label to treat a number of other skin conditions, such as squamous cell carcinoma despite strong evidence.

Victor Desmond Mandel, M.D. and colleagues describe a reconstruction strategy for chronic infected neoplastic ulcers of the lower extremities using a dermal matrix and a unique postoperative dressing protocol.

Squamous cell carcinoma in hidradenitis suppurativa is rare, but mortality is high, according to Mayo Clinic researchers reporting at the American Society for Dermatologic Surgery annual meeting last week in Phoenix.
The new AAD cSCC treatment guidelines highlight alternative therapeutic or preventive treatment options.

Dermatofibrosarcoma protuberans (DFSP), dermatofibromas, keloids and hypertrophic scars are four separate conditions requiring assessment, but only one requires a biopsy.

In this quiz, Kaivon Sobhani, B.S., and, Eve Lowenstein, M.D., Ph.D., FAAD, address dermatofibrosarcoma protuberans (DFSP), keloids, hypertrophic scars and dermatofibromas.

Studies have shown that melanoma incidence rates among non-Hispanic whites have been rising in recent years, which is true ― to a degree, according to a research letter published in March in JAMA Dermatology. The rates are indeed rising for those younger than 15 years old and older than 45 years old. However, the analysis highlights a big dip in melanoma cases for those between 15-44 years.