TRuE-AD1 and TRuE AD2 Trial Overview
Dermatology experts review the design of the TRuE-AD1 and TRuE AD2 phase 3 trial.
Episodes in this series

James Q. Del Rosso, DO: We’re going to talk about the timing and magnitude of the effect of ruxolitinib [Opzelura] cream on itch in patients with atopic dermatitis, which produces an inflammatory eczematous dermatitis in almost every patient associated with significant itching. There were 2 phase 3 trials, which enrolled patients who were at least 12 years of age. They had a diagnosis of atopic dermatitis for at least 2 years, and they had an Investigator Global Assessment score of 2 or 3 as a baseline, which means that the investigator utilizing criteria based on the study rated them as mild or moderate.
The majority of the subjects looked at in the trial were moderate severity, but it also included mild. The body surface area [BSA] involvement was anywhere from 3% to 20%. The scalp was excluded in that assessment. These trials were called TRuE AD1 and TRuE AD2, which are 2 parallel, double-blind, vehicle-controlled trials with different investigators in different subjects.
As far as exclusions in the studies, subjects were ineligible if the investigator determined that they had an unstable course of atopic dermatitis, which could quickly improve or deteriorate because it’s hard to assess that in terms of what the medication would be doing. Other types of eczematous dermatitis or significant immunocompromised can influence the evaluation of the patient and any other type of treatment during the designated washout periods. When patients enter the study, we don’t want them utilizing other things that can influence the results. We want the patient at baseline to be in a stable state, so we can evaluate whether they’re responding to the ruxolitinib cream or the vehicle cream.
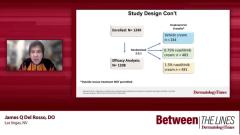
A total of 1249 patients were enrolled in the study, and the efficacy analysis included 1208 patients. These were subjects who had utilized at least 1 application of the medication. They were randomized 2 to 2:1, which means you had 483 patients treated with ruxolitinib cream 0.75% or 481 patients treated with 1.5% ruxolitinib cream. Compare this with the vehicle cream. You need to have enough in the vehicle arm so you can get a statistical analysis. There were 244 patients treated over a period of 8 weeks.
Keep in mind, nobody knew what group they were in. They didn’t know if they were applying a vehicle cream or either percentage of ruxolitinib cream. If they started with the 1.5% cream, that was utilized throughout the study. But the investigators, staff, and patients in the study didn’t know exactly what they were getting; it was blinded. No rescue treatment was allowed, so they couldn’t use some therapeutic agent, a topical corticosteroid, or a calcineurin inhibitor if they weren’t adequately controlled. This looked only at ruxolitinib vs the vehicle cream.
Raj Chovatiya, MD, PhD: You’re no stranger to clinical trials. Is itch a important end point for you? Is it 1 of those throw-ins: “That’s fine. It’s not the primary end point?” Or does that matter when you’re looking at data?
Lisa Swanson, MD: It’s very important because itch improvement is happiness elevation. There’s an inverse relationship between itch and happiness. The less itch you have, the more happiness you’re going to have. That’s very meaningful to me.
Raj Chovatiya, MD, PhD: I wish we had the Swanson happiness index as a clinical trial measure. In the absence of that, it’s important to think about any way we can measure itch. Sometimes we’re bound by these end points that regulatory bodies want for a label. But in the clinic, from a day-to-day perspective, I want to ask patients, are you feeling less itchy? Do you feel better? That’s what seals the deal when something is working for them.
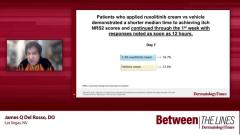
Given everything we’ve talked about, the new ways we have to think about itch is what excites me when it comes to atopic dermatitis. There’s a huge burden. Everybody wants their itch gone yesterday. Speed is an important part in addition to magnitude. In the recent clinical trial programs, TRuE AD1 and TRuE AD2, they looked at 1.5% ruxolitinib cream, which is approved for children and adults. They tried to take a deeper dive into understanding some of that timing and magnitude when it came to itch relief.
This was a trial program, with a parallel phase 3, and individuals were all 12 years and up. They had atopic dermatitis for a couple of years, usually mild and moderate disease. This is very appropriate for topicals, and that’s largely what we’re thinking about in that group. There’s an important caveat, and I’d love to hear your thoughts. This was designed to think about patients who had 3% to 20% body surface area. When I think about my patients that who have mild and moderate disease, that sweet spot is around 10%, where it’s practical for them to use topicals.
Lisa Swanson, MD: I agree 100%. That was very appropriately set up. That’s an appropriate BSA involvement to study for topical medication.
TRANSCRIPT EDITED FOR CLARITY
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.