Ruxolitinib: Clinical Context
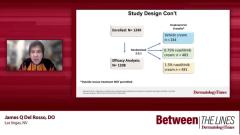
Raj Chovatiya, MD, PhD, Lisa Swanson, MD, discuss take a closer look at the TRuE-AD1 and TRuE AD2 phase 3 trial and provide context regarding ruxolitinib cream for the treatment of atopic dermatitis in the clinical setting.
Episodes in this series

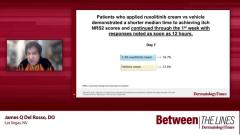
Raj Chovatiya, MD, PhD: When you parse this out into common end points that we use, we don’t think a 2-point improvement on that NRS [Numeric Rating Scale] sets the bar a little higher. It’s not just any kind of improvement. And when you do that analysis, you see, at that 1.5% concentration that’s approved, day 1, within 12 hours, you’re seeing a separation. So already within hours, you’re seeing people feeling better. Does this reflect what you’ve seen in your practice?
Lisa Swanson, MD: It really does. I have found that topical ruxolitinib [Opzelura] works with the speed of a topical steroid without being a topical steroid. And that’s one of my favorite things about it is the rapid onset of action, rapid onset of relief for the patient.
Raj Chovatiya, MD, PhD: What’s interesting is that this is also one of the few circumstances I can think of in recent memory where what I saw in terms of the numbers has reflected what I feel my patients tell me, too.
Lisa Swanson, MD: 100%. Definitely.
Raj Chovatiya, MD, PhD: There are not that many times that people message me with good news or call me with good news, but I feel I got a handful of those when I had a chance to use it in the clinic. And that was a really big moment for me to put in context how the speed of resolution of itch was really important to patients.
Lisa Swanson, MD: Absolutely. And it also leads to practical advice because if you give a patient a sample of topical ruxolitinib, that sample will last them maybe a day or 2 or 3 or 4. But this data shows that that would be meaningful to show improvement so they could get a taste of what they can expect.
Raj Chovatiya, MD, PhD: That’s a really cool way to think about it. And when you follow out some of that data just thinking about 2 points of improvement, really whether you’re looking at week 2, week 4, week 8, which were the visit study end points people looked at, you were already seeing people achieving control and the majority of folks got to where you wanted to get them to at the week 8 time point.
Now, when you raise that bar a little bit and start thinking about a 4-point improvement. I know I was a little tongue-in-cheek railing on some of those regulatory end points, but that 4-point improvement is oftentimes what the agency wants to see when it comes to getting something approved. And if you take that as a standard within 36 hours, you start to see a statistically significant separation between the vehicle and treatment. So really a higher bar still is talking about hours here as opposed to even days, which is pretty incredible.
Lisa Swanson, MD: It’s amazing. Ten percent of the patients were already achieving itch improvement greater than or equal to 4 by day 2. That’s super impressive for a topical medication.
Raj Chovatiya, MD, PhD: When you follow that out to 8 weeks as well, what you end up seeing is that the majority of patients are getting to that itch end point, which it’s difficult for me to think of other examples where I get to say the majority of patients achieved something in a trial. Because we’re always talking about 15%, 20%, 25%, but to say more than 50% of patients. I can tell my patients that based on what I saw on the trial, you have a really good chance of getting your itch controlled.
Lisa Swanson, MD: I think roughly by the end of the study, by week 8, a little bit more than half [of the patients] had achieved itch improvement greater than or equal to 4.
Raj Chovatiya, MD, PhD: I know that we’ve been bouncing around to different ways to think about improvement, whether it’s any improvement, a couple of points, or 4 points. We didn’t really spend any time talking about 3 points of improvement, but there are a lot of studies out there that really say that if you get people better, these are probably very meaningful to patients. And I can’t say enough that we’re oftentimes so beholden to the data that’s on a label or data that are presented to us in a deck or a conference or what we see in the pivotal phase 3 paper that sometimes we forget that real-life clinical practice is a little different. And maybe we’re not making these measurements in this way. But really, if you’re just using your gestalt, if you will, that someone is doing better, that’s really the most important thing that matters.
Lisa Swanson, MD: The studies help guide us and choose medications appropriate for our patient population. But it’s really the patient response in that clinic exam room that’s the most meaningful to us.
Raj Chovatiya, MD, PhD: I think one of the nice things about having the opportunity to look at the data and have data that represents a pretty broad demographic subset of people and understand that when you cut this out further, there didn’t seem to be any difference between some of those major socio-demographic groups that we like to look at, whether we’re talking about white vs. nonwhite, whether we’re talking about gender differences, whether we’re talking about other aspects of treatment in terms of previous treatment experience. And I think that’s really relevant to real-life practice where there is a huge diversity of patients. Aside from just diverse skin types, both in terms of how they look, how they behave, and how people choose to identify, that’s really the most important thing. And knowing that oftentimes the biggest challenge is getting our patients to come and see us. I feel that if that’s the biggest challenge we have with this particular treatment, that’s a pretty good challenge.
Lisa Swanson, MD: Oh, 100%. We like to see consistently effective therapies for our patients, regardless of all the factors. And I think we see that with this data.
Raj Chovatiya, MD, PhD: Let me ask you a question because you probably have some thoughts as well. Did you used to think about the rapidity of onset of treatment as something important? And have your thoughts changed on this at all since we have options where we can talk about that stuff?
Lisa Swanson, MD: I think rapidity of onset of action has always been important. There have been some therapies over the years that haven’t been able to achieve that. And so, we got comfortable accepting that. But now we have all these therapies that can work fast. And that’s really what our patients want.
Raj Chovatiya, MD, PhD: I got to say, I feel it’s not something I probably emphasized and talked about and asked all that much because usually, I was very used to saying, “OK, in 3 months, 4 months, check back in, see how things are going.” But when you ask somebody about if it matters if what I choose works quickly, I feel like they tell me, “I want this itch gone now. I want it gone yesterday. Give me whatever works the quickest.” And so, with anything, the fact that we can measure changes this quickly and change that narrative and dialogue and spin it around makes me feel like we have the ability to maybe even change how we approach that therapeutic decision-making with our patients.
Lisa Swanson, MD: I think if we gave patients a choice between a medicine that could make their itch better in a week vs. a medicine that could make their itch better in 3 weeks, 100% of them would choose the 1-week itch relief medicine.
Raj Chovatiya, MD, PhD: And to even build off that, the entire landscape is shifting in atopic dermatitis. And so just with topical therapy, this is one of probably others that are going to be coming out that we have opportunities to use. We’ve seen some big movement in the systemic therapy space, both in terms of biologic therapy, but also oral JAK [Janus kinase] inhibitors. And the interesting thing about the oral JAK inhibitors is you end up seeing very similar types of comparisons with the rapidity of onset. And I think it’s just another piece of evidence that’s really told us that that matters to our patients.
Lisa Swanson, MD: Oh, 100%. And I think that’s one of the best things about these JAK inhibitors, whether it’s topical or oral, is their speed of onset, very fast.
Raj Chovatiya, MD, PhD: In this mild-to-moderate group with topical ruxolitinib of your patients, how is it fitting in with that right patient when you’re trying to match up a therapy with somebody?
Lisa Swanson, MD: I love topical ruxolitinib. And I tell patients that I love it because it works as well and as fast as a topical steroid without being a steroid. It’s what we have been waiting for for decades. And so, I think the only thing that holds me back is have they checked all the boxes from the insurance company in order to get coverage for the topical ruxolitinib? A lot of insurance companies will require a failure of a topical steroid or a TCI [topical calcineurin inhibitor]. So as long as I've checked those boxes, I’m on board with recommending this to my patients. And they really like it.
Raj Chovatiya, MD, PhD: I couldn’t put it better. I think this is one of those things that’s been a home run for discussing with patients that are the appropriate ones. And I think identifying the right patient is key because you need somebody that has reasonable severity but also not extraordinarily extensive disease just for the practicality of applying a topical as well. I think that this is going to have a huge impact on that patient population, those tweeners, if you will, that you could think about a systemic therapy, but you wish that you had a better option than a topical steroid and maybe it is going to help us come to a day where we don’t have to think about topical steroids even.
Lisa Swanson, MD: Oh, my gosh. Can you imagine? Wow. That would be amazing.
Raj Chovatiya, MD, PhD: We use them, and we talk about them to any dermatologist. No one loves having to use topical steroids because of the worry of, well we can’t use them for that long. We might have pigmentary issues. You could have thinning of the skin. You might end up with some long-term stretch mark-looking stuff. It’s especially concerning with kiddos. They end up using them for years and years and years. And there’s data to suggest that that stuff can cause systemic effects, changes in bone health, and even growth.
Lisa Swanson, MD: I think our lack of options in the past and the cheapness of topical steroids have led to them being used quite frequently. A lot of times we just had nothing else. But that world is changing in a very exciting way.
TRANSCRIPT EDITED FOR CLARITY
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.