- General Dermatology
- Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
Mastering the Challenges of Adult Female Acne in Primary Care in 2024
Over 50% of women in their 20s and over 35% of women aged 30 to 39 years struggle with adult female cystic acne.
The Hidden Battles of Adult Female Acne
Ocskay Bence/AdobeStock

Acne vulgaris, a relentless adversary, casts its shadow over the lives of countless adult females. For Sarah, aged 30, the battle is not merely skin-deep; it is an emotional odyssey. The painful cysts deep within her skin throb with a constant reminder of her struggle. They are more than just a physical burden; they are a symbol of the emotional turmoil that plagues her daily existence.
The mirror, an unflinching truth-teller, reveals the scarlet constellations of cyclical acne that have, over time, etched a map of silent battles across her cheeks and jawline. She faces a daily confrontation with a myriad of emotions: frustration at the persistence of such a condition past the turbulent years of adolescence, embarrassment that prompts a reflexive turn of the head or a sweep of hair to obscure the skin's story, and a gnawing self-consciousness that permeates interactions, both personal and professional. This relentless cycle, marked by the ebb and flow of flare-ups, challenges her sense of identity and self-esteem.
Sarah is not alone in her fight. Over 50% of women in their 20s and over 35% of women aged 30 to 39 years struggle with adult female cystic acne, impacting their well-being dramatically.1 Despite being the eighth-most prevalent disease in the world, acne is still often perceived as a teenage affliction.2 This misconception leaves adult sufferers like Sarah grappling with poor self-esteem, stigmatization, bullying, depression, anxiety, and even suicidal ideation.3
Conquering Adult Female Acne in Primary Care
As primary care providers, we stand at the forefront of the dermatological landscape, bearing witness to the unspoken pain etched upon the faces of our patients. Acne affects countless lives, but for women, it cuts deeper. We have the power to not only treat acne but to restore confidence and transform lives. By understanding the unique challenges of adult female acne and implementing the latest guidelines, we can become the beacons of hope our patients need.
The 2024 American Academy of Dermatology (AAD) acne guideline update brings significant changes, particularly in the realm of adult female acne treatment. This includes the first-in-class topical antiandrogen treatment for acne vulgaris, clascoterone cream 1%, a topical androgen receptor inhibitor approved for patients 12 years and older.4 The ability to topically block androgen production has been on the wishlist for dermatology providers for decades, as it is one of the key drivers in adult female acne. Previously, there have only been oral options, such as spironolactone and combined oral contraceptives (COCs). With the new guidelines, primary care providers can now more easily initiate treatment for their patients battling adult female acne.
Hormonal Acne and Menstrual Cycle: What's the Link?
Figure. Acne pathophysiology
Credit: Michael Rubio, PA-C
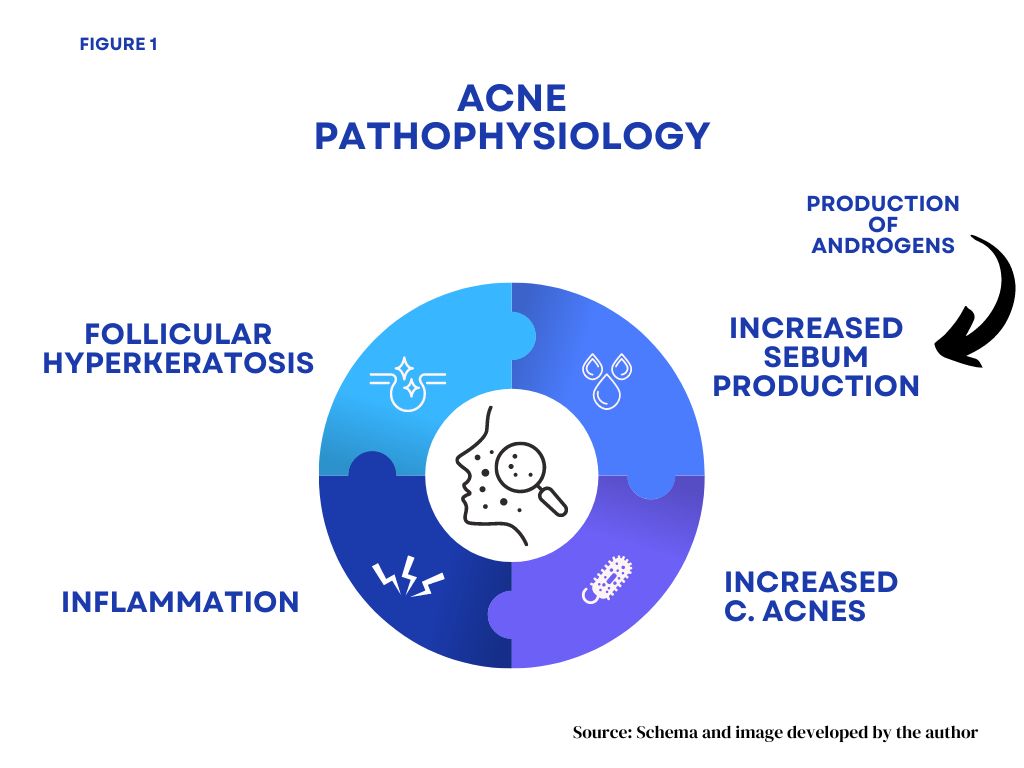
Adult female acne is frequently referred to as "hormonal acne." However, the term "hormonal acne" for adult female acne is a misnomer, as all acne is hormone-mediated. "Cyclical" or "premenstrual" acne would be more appropriate terms since acne in adult females often fluctuates with the menstrual cycle.5 Adult female acne, like all acne, as noted in the Figure, is driven by fluctuations in androgen levels that lead to increased oil (sebum) production, clogged pores (follicular hyperkeratinization), increased Cutibacterium acnes (C. acnes) bacteria, and inflammation.
Adult female acne classically presents as deep, painful cysts along the lower parts of the face, upper chest, and back, but it can involve multiple facial areas and mixed comedones as well.6 Identifying adult female acne requires a thorough patient history, including menstrual cycle patterns, medications, and social and family history. The key descriptor in the history is "persistent," which was noted in 75% to 85% of cases.7 Lastly, it is important to remember that persistent acne in a woman can also indicate a systemic disease, such as polycystic ovary syndrome (PCOS), which is associated with hormonal and metabolic disorders.
Adult Female Acne Therapies: How Long Before Patients See Results?
Treatment success means that the care plan integrates well with the patient's existing skincare routine, personal preferences, and treatment goals. The bulk of the work will be in partnering with your patient and managing expectations. Some may want to start slow, some may be opposed to COCs, and some may have no clue at all; all of the above are normal. Our main goal is to keep our patients safe and informed.
It is good practice to set treatment endpoints. All acne clinical trials are conducted for 12 weeks, so if progress is not seen or the end goal is not met within that timeframe, strongly consider changing plans, stepping up treatment, or referring the patient to a specialist. Waiting past 3 months without any improvement, especially if the patient is already on a topical retinoid, benzoyl peroxide, and an oral antibiotic such as doxycycline, may delay clearance, exacerbate antibiotic resistance, and prolong the patient's condition.
Topical Treatments for Adult Female Cystic Acne
For many women, inhibiting androgen production is the key to sustained clear skin, as it is the main driver in adult female acne. A comprehensive discussion of all anti-androgen agents is beyond the scope here, but there are three appropriate options: COCs, spironolactone, and clascoterone. The only topical anti-androgen inhibitor to date is clascoterone, which is one of the most important updates to treating adult female acne in primary care. The AAD 2024 acne guideline noted the benefits of this novel treatment but cited concerns over its current high cost.8
When to Refer
Not all cases of adult female acne can be handled in a primary care setting, which is why it is important to familiarize yourself with when to refer. Per the guidelines, consider referring patients with severe acne, acne-causing psychosocial burden or scarring, or acne failing standard treatment with oral or topical therapy to a dermatology provider. In cases like these, initiation of isotretinoin therapy is usually advised. In addition, if you have tried the first-line treatments and there has been no improvement after approximately 6 months, it may be time to reach out to a specialist.
Summary
In summary, adult female acne is a multifaceted condition that requires a holistic, empathetic, and evidence-based approach from the frontline primary care providers. The advent of topical antiandrogen treatments, such as clascoterone, marks a significant advancement in our capacity to address a key factor in adult female acne: topical androgen inhibition. However, our responsibility goes beyond simply writing prescriptions. We must collaborate with our patients, incorporating their needs and objectives into a holistic treatment plan that tackles both the physical and psychological facets of this condition.
Michael Rubio, PA-C, is a dermatology physician assistant at Infinity Dermatology in Brooklyn, NY. He is the Vice Co-Chair of the Society of Dermatology Physician Assistants Communication Committee and a contributor to the National Commission on Certification of Physician Assistants development of the Certificate of Added Qualifications in Dermatology. He is also a co-founder of Well Revolution (www.wellrevolution.com), a same-day direct primary care platform helping to address the primary care shortage crisis in the United States.
References
- Collier CN, Harper JC, Cafardi JA, Cantrell WC, Wang W, Foster KW, Elewski BE. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008 Jan;58(1):56-9. doi: 10.1016/j.jaad.2007.06.045. Epub 2007 Oct 22. Erratum in: J Am Acad Dermatol. 2008 May;58(5):874. Cafardi, Jennifer A [added].
- Moradi Tuchayi S, Makrantonaki E, Ganceviciene R, Dessinioti C, Feldman SR, Zouboulis CC. Acne vulgaris. Nat Rev Dis Primers. 2015 Sep 17;1:15029. doi: 10.1038/nrdp.2015.29.
- Hebert A, Thiboutot D, Stein Gold L, et al. Efficacy and safety of topical clascoterone cream, 1%, for treatment in patients with facial acne two phase 3 randomized clinical trials. JAMA Dermatol. 2020;156(6):621-630. doi:10.1001/jamadermatol.2020.0465
- Shields A, Nock MR, Ly S, Manjaly P, Mostaghimi A, Barbieri JS. Evaluation of stigma toward individuals with acne. JAMA Dermatol. 2024;160(1):93–98. doi:10.1001/jamadermatol.2023.4487
- Dréno B, Thiboutot D, Layton AM, Berson D, Perez M, Kang S. Global Alliance to Improve Outcomes in Acne. Large-scale international study enhances understanding of an emerging acne population: adult females. J Eur Acad Dermatol Venereol. 2015;29:1096-106.
- Zeichner JA, Baldwin HE, Cook-Bolden FE, Eichenfield LF, Fallon-Friedlander S, Rodriguez DA. Emerging issues in adult female acne. J Clin Aesthet Dermatol. 2017 Jan;10(1):37-46. Epub 2017 Jan 1.
- Dumont-Wallon G, Dréno B. Specificity of acne in women older than 25 years. Presse Med. 2008 Apr;37(4 Pt 1):585-91. French. doi: 10.1016/j.lpm.2007.07.014. Epub 2008 Mar 7. .
- Reynolds RV, Yeung H, Cheng CE et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2023. doi:10.1016/S0190-9622(23)03389-3.

