- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
News
Article
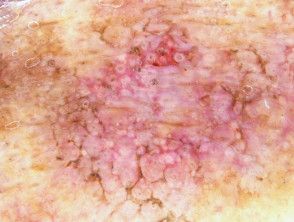
Phase 1 Maximal Use Trial of Tirbanibulin Ointment 1% in Actinic Keratosis Exhibits Favorable Safety and Tolerability
Author(s):
The study explored the use of the ointment in an area of 100 cm squared.
Tirbanibulin ointment 1%, a synthetic tubulin polymerization and Src kinase signaling inhibitor, has demonstrated efficacy in smaller fields wherein actinic keratosis (AK) lesions are located. Currently, it is approved in the United States and Europe with efficacy and safety data supporting its use when applied to a field of up to 25 cm2.
In a phase 1 maximal-use trial exploring the plasma pharmacokinetics, safety, and tolerability of tirbanibulin on a 100 cm2 field, researchers presented data supporting its potential use in larger affected areas.
This multicenter, open-label, phase 1 trial enrolled 28 adult patients with AK between July 15, 2021, and October 19, 2021.
Patients were instructed to apply tirbanibulin ointment 1% daily to a 100 cm2 field on the face or balding scalp for 5 days. Pharmacokinetic parameters, safety, and local tolerability were assessed, and patients were followed up for 29 days.
As a result, researchers found that tirbanibulin plasma exposure was fourfold higher than previous studies with a 25 cm2 field, indicating dose-dependent systemic absorption.
On day 5 of the study, the average maximum plasma concentration was 1.06 ng/mL, and area under the curve was 16.2 ng h/mL. Accumulation ratios from day 1 to the last treatment day were 1.94 for the face and 2.77 for the scalp.
In addition, tirbanibulin applied to a 100 cm2 field exhibited favorable safety and tolerability.
The most common treatment-emergent adverse events were application site reactions in 35.7% of patients, all of which were mild to moderate in nature and resolved by day 29. No serious adverse events or adverse events of special interest were reported.
Local tolerability signs, including erythema, flaking/scaling, crusting, swelling, vesiculation/pustulation, and erosion/ulceration, were generally mild and transient in nature. Composite scores indicated manageable tolerability.
The favorable safety profile, manageable local tolerability, and minimal systemic exposure observed in this trial align with tirbanibulin's established efficacy in smaller fields, study authors wrote. These findings support tirbanibulin's potential use in treating larger areas affected by AK, addressing the need for field-directed therapies.
Potential study limitations included its small sample size and high pharmokinetic (PK) variability. Additionally, the sample of patients involved in the study was more reflective of a population of typical patients with AK (older, male) than the general population.
"The PK and safety of tirbanibulin ointment 1% were well characterized in patients with 8 or more clinically typical, nonhypertrophic, nonhyperkeratotic AK lesions in a field of 100 cm2, and the current data support the safety of tirbanibulin ointment 1% when applied to a larger surface area, beyond the 25 cm2," study authors wrote. "The results of this Phase 1 study show tirbanibulin's tolerability and safety are good and adequate to consider it a suitable therapeutic option, compared to other treatments, such as imiquimod or 5-fluorouracil. The present data support the conduct of a larger Phase 3 safety and efficacy study in a large field."
Reference
DuBois J, Jones TM, Falqués M, et al. Pharmacokinetics, safety, and tolerability of a single 5-day treatment of tirbanibulin ointment 1% in 100 cm2: A phase 1 maximal-use Trial in patients with actinic keratosis. Clin Pharmacol Drug Dev. Published January 7, 2024. Accessed January 10, 2024. https://doi.org/10.1002/cpdd.1368