- General Dermatology
- Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
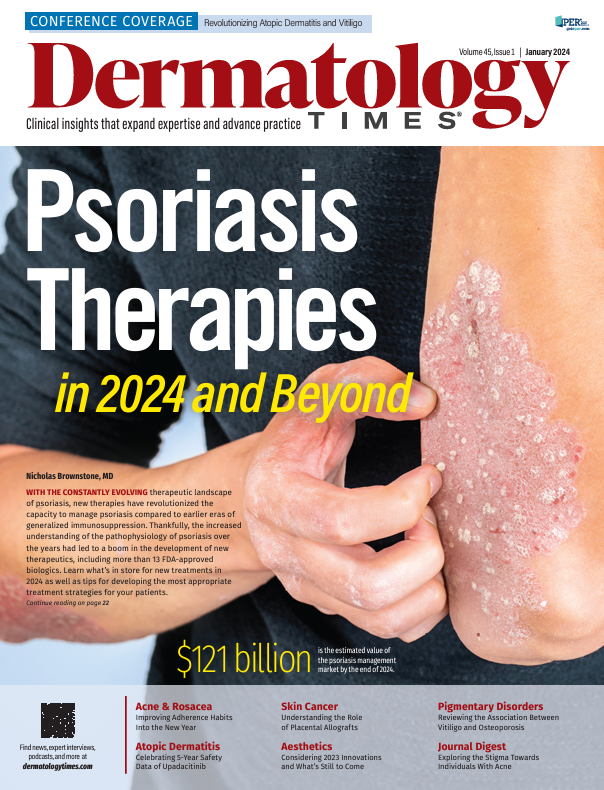
Psoriasis Therapies in 2024 and Beyond
This article will highlight recently approved psoriasis therapies that will shape the 2024 treatment landscape and provide some exciting updates in the psoriasis management market this coming year and beyond.
Decades ago, psoriasis was still primarily considered a problem with hyperproliferation of the epidermis. Given the antiquated understanding of this disease pathophysiology, traditional oral immunosuppressive agents were used for moderate to severe presentations. Recent research into the pathophysiology of psoriasis has highlighted the importance of the immune-mediated nature of this very common inflammatory skin disease. There now exists a clear mechanism down to the molecular level regarding which cytokines are implicated in the pathophysiology of psoriatic disease. When considering these different molecular signaling pathways, IL-23–mediated activation of the Th17 pathway is hypothesized to be the main contributor to the inflammation seen in psoriasis.1 Due to its important role in the pathophysiology of psoriasis, IL-23 has been referred to as the master cytokine in psoriatic disease by many clinicians and researchers. Other important cytokines include TNF-α and IL-17. The fact that biologic agents interact with a specific cytokine (such as TNF-α, IL-17, or IL-23) in a targeted manner has revolutionized the capacity to manage psoriasis compared with the era of a more generalized immunosuppression reflected by the traditional oral medications (eg, methotrexate, cyclosporine, and acitretin). This represents an improved treatment paradigm where targeted immunomodulation has resulted in a great enhancement in both safety and efficacy for the biologic agents.
There are now more than 13 FDA-approved biologic options for moderate to severe psoriasis. Additionally, there have been new approvals for oral and topical therapies for psoriasis, including a topical first-in-class mechanism of action for psoriatic skin lesions. Given that psoriasis affects more than 7 million adults in the US, the therapeutic landscape is constantly evolving.2 It is estimated that the psoriasis management market will be worth nearly $121 billion by the end of 2024.3 This article will highlight recently approved psoriasis therapies that will shape the 2024 treatment landscape and provide some exciting updates in the psoriasis management market this coming year and beyond. It will also highlight how biosimilar medications will affect the field for years to come and cover new updates in the management of pediatric psoriasis.
Biologics
The newest biologic agent for psoriasis, bimekizumab (Bimzelx), was approved by the FDA on October 18, 2023, for the management of moderate to severe psoriasis. Bimekizumab is unique in that it blocks both the IL-17A and IL-17F cytokines. The other IL-17 antagonists approved to manage psoriasis either only block IL-17A (ixekizumab and secukinumab) or block the IL-17 receptor (brodalumab). In findings from the phase 3 BE READY trial (NCT03410992), which studied bimekizumab in the management of moderate to severe psoriasis, 91% of 349 patients receiving this medication at 320 mg every 4 weeks achieved a Psoriasis Area and Severity Index (PASI) score of 90 compared with 1% of 86 patients receiving placebo.4 In findings from the phase 3 BE OPTIMAL trial (NCT03895203), which studied bimekizumab in the management of psoriatic arthritis (for biologic-naive patients), significantly more patients receiving bimekizumab (44%) reached American College of Rheumatology 50% response vs those receiving placebo (10%).5 “Head-to-head studies with bimekizumab vs currently FDA-approved biologic agents, including adalimumab, secukinumab, and ustekinumab, have highlighted the rapid onset of action of this new biologic medication. Even before the second dose, this is a significant PASI response, making this a great option for a patient whose main concern is rapid improvement with infrequent dosing compared with some competitors. Bimekizumab’s unique mechanism of action [IL-17A/F] is a novel and exciting addition to the current biologic landscape for psoriasis,” G. Michael Lewitt, MD, FAAD, a board-certified dermatologist at Rosealind Franklin-Chicago Medical School in Chicago, Illinois, said.
Pooled safety analysis from phase 2 and phase 3 showed that nasopharyngitis, oral candidiasis, and upper respiratory tract infection were the most common treatment-emergent adverse events reported with bimekizumab. IL-17 is involved in mucosal host defenses against fungal infections; therefore, anti–IL-17 biologics can be associated with an increased risk of oral mucocutaneous candidiasis.6 Of the patients in the phase 2/3 trials, 15.4% reported an oral candidiasis event in the first year and 9.1% reported it during the second year. These rates are higher when compared with the other IL-17 antagonists.
Although not considered a new biologic, adalimumab will greatly affect the 2024 psoriasis treatment landscape because generic versions are approved for the management of adult plaque psoriasis. These include the 9 following FDA-approved agents: adalimumab-aacf (Idacio), adalimumab-fkjp (Hulio), adalimumab-adbm (Cyltezo), adalimumab-bwwd (Hadlima), adalimumab-adaz (Hyrimoz), adalimumab-aaty (Yuflyma), adalimumab-aqvh (Yusimry), adalimumab-afzb (Abrilada), and adalimumab-atto (Amjevita).7 According to the FDA, biosimilars must prove bioequivalence and be tested by way of clinical trials to ensure they will exhibit no significant differences to their parent product.8
Two adalimumab (Humira) biosimilars—adalimumab-adbm and adalimumab-afzb—carry interchangeable status, whereas the others still need to undergo testing. These 2 specific medications underwent additional testing to be granted this status, including a switch study. A switch study is one where patients alternate between taking adalimumab and a biosimilar multiple times. This type of study supports similarity between agents, with no changes in patient clinical status when a biosimilar is substituted for the original medication (and vice versa).9 A recent systematic literature review found that switching between reference adalimumab and biosimilars has no impact on efficacy, safety, and immunogenicity in patients with rheumatoid arthritis, psoriasis, and inflammatory bowel disease.10 The 4-letter suffixes that are now required to be assigned to biologic agents are very important to appreciate because they allow both practitioners and patients the ability to identify different biologic products without confusion and to prevent the inadvertent substitution of biological products that have not been deemed interchangeable. There will be challenges to effective adaptation and integration of biosimilars into everyday practice. These potential issues may include differences in package sizes, injection devices, inactive ingredients, dosing regimens, and patient preference for the brand name Humira. The pharmacy benefit managers, especially the 3 largest ones—Optum Rx, CVS Caremark, and Express Scripts—are going to have a powerful influence on the distribution of the adalimumab biosimilars by means of their formularies. For example, Optum Rx has announced that it is putting adalimumab-adbm, adalimumab-adaz, and adalimumab-atto on its formulary.11
Topicals
In terms of new and exciting topical therapies for patients with psoriasis, roflumilast cream was approved by the FDA in 2022 for management of plaque psoriasis in adults and adolescents. Roflumilast is a topical PDE4 inhibitor. PDE4 degrades its substrate cyclic adenosine monophosphate (cAMP) to adenosine monophosphate (AMP), which leads to the production of proinflammatory mediators. Therefore, inhibitors of PDE4 work by blocking the degradation of cAMP, which leads to a reduction in inflammation.12 Inhibitors of PDE-4 work by blocking the degradation of cAMP, which leads to a reduction in inflammation. Roflumilast is the only topical treatment for which efficacy has been specifically demonstrated in the management of intertriginous psoriasis.13 Intertriginous psoriasis is typically difficult to manage topically given the relative contraindication of superpotent topical steroids.
Looking ahead to 2024 and beyond, roflumilast is being studied for approval as a foam formulation for the management of scalp and body psoriasis. Foam formulations can be applied through the hair more easily to manage lesions more effectively on the skin of the scalp and other large hair-bearing areas. Results from a phase 2b study recently published in the British Journal of Dermatology found that significantly more patients treated with roflumilast foam (59.1%) vs patients treated with vehicle (11.4%) achieved secretory IgA success at week 8, with differences detected as early as week 2 for scalp and body psoriasis.14 Roflumilast foam is also being studied for the management of seborrheic dermatitis, a common condition seen in dermatology clinics that lacks a large array of effective therapies. Findings from another recent phase 2a randomized controlled trial published in JAMA Dermatology showed that once-daily roflumilast foam demonstrated favorable efficacy, safety, and local tolerability in the management of erythema, scaling, and itch caused by seborrheic dermatitis.15 Given that seborrheic dermatitis mostly involves the scalp, having an FDA-approved foam vehicle for treatment would be welcomed by many clinicians. “Roflumilast foam is currently pending FDA approval for seborrheic dermatitis. Many clinicians use the diagnosis sebopsoriasis, which indicates an overlap between seborrheic dermatitis and scalp psoriasis. Foams are often ideal vehicles for hair-bearing areas, so roflumilast foam will be an excellent topical choice in these patients,” Lewitt said.
[Update: Roflumilast foam 0.3% for seborrheic dermatitis was approved by the FDA on December 15, 2023, prior to print publication.]
Pediatric Solutions
For pediatric psoriasis, where there have been traditionally fewer options for treatment, new therapies are needed. Currently, there are systemic agents approved by the FDA to manage pediatric psoriasis, but they are biologic therapies that require subcutaneous injections, which may be unappealing to pediatric patients. Apremilast, an oral systemic therapy approved by the FDA in adults for mild, moderate, and severe psoriasis, is currently being studied for pediatric psoriasis. Results from a phase 3 study investigating the efficacy of apremilast in pediatric patients aged 6 to 17 years found that the medication was well tolerated and effectively reduced psoriasis severity in patients aged 6 to 17 years.16 Data from the phase 3 SPROUT trial (NCT03701763) are encouraging and could provide a valuable and attractive alternative to biologic therapy for pediatric patients who require systemic therapy or who have psoriatic arthritis. The adverse events were consistent with the known safety profile of apremilast in pediatric patients, with the most commonly reported (at least 5% of patients) in either treatment group being diarrhea, headache, nausea, and nasopharyngitis.17
Recently approved topical therapies for pediatric psoriasis includes roflumilast cream, which just received FDA approval in October 2023 for pediatric patients 6 years or older.18 This is exciting news because there were no previously FDA-approved nonsteroidal topical therapies approved for pediatric patients younger than 12 years. Many parents and clinicians are cautious and wary of topical corticosteroids for the management of psoriasis in pediatric patients given the risk of irreversible skin striae and skin atrophy associated with long-term topical steroid use. Given that psoriasis is a chronic disease and many pediatric patients have only mild disease that is easily managed with topical therapy, a nonsteroidal topical option is very attractive to both clinicians and pediatric patients because of the nonexistent risk of skin striae and skin atrophy. Furthermore, roflumilast cream is an ideal topical therapy for pediatric patients because it may be used on any skin site, for any severity of disease, and with no limitation on duration or use. There are no warnings or contraindications in the FDA package insert (with the exception of the fact that it should be avoided in patients with moderate to severe liver impairment).Liver impairment is extremely rare in pediatric patients, so in clinical practice, there are essentially no relative or absolute contraindications for the use of roflumilast cream for the management of pediatric psoriasis.
Looking Ahead
This coming year will certainly be an exciting one for the management of psoriasis. Despite the rapidly evolving therapeutic armamentarium for the management of psoriatic disease, unmet needs still unfortunately remain. Nail psoriasis has been notoriously difficult to manage, so more effective therapies are desperately needed. Furthermore, cost and access for these novel therapies could be improved as well. New research is beginning to focus on developing therapies using biomarkers and personalized medicine to mitigate treatment failures and adverse events when using systemic therapies.19 This personalized medicine approach may identify super responders, who are patients who may require less frequent dosing or smaller doses of medication to achieve clearance.20 Biomarkers for psoriasis are being investigated to also aid in the diagnosis of psoriasis.
Resident memory T cells in the pathogenesis of psoriasis are being studied to possibly mitigate future psoriasis flares through knockout therapy. This is based on the theory that if one manages psoriasis earlier, when patients are just diagnosed, one might be able to decrease resident memory T cells that are created in the skin and are responsible for future flares.20 At least 2 companies are developing a peptide-type small molecule that blocks IL-17 and IL-23 signaling and is given as an oral systemic agent, possibly ushering in a new era of oral biologics. Another concept that is being studied is an oral systemic agent that protects a biologic agent from digestion in the gastrointestinal tract and autoinjects into the wall of the small intestine.21
Lewitt weighed in on what he is most excited for in 2024 for the management of psoriasis. “Some exciting innovations in the psoriasis [management] landscape in 2024 are the phase 3 trials for an oral IL-23 inhibitor and new phase 4 data on [management] of head and neck psoriasis with topical tapinarof,” he concluded.
Nicholas Brownstone, MD, is a dermatology resident at Temple University Hospital in Philadelphia, Pennsylvania.
References
- Alwan W, Nestle FO. Pathogenesis and treatment of psoriasis: exploiting pathophysiological pathways for precision medicine. Clin Exp Rheumatol. 2015;33( 93):S2-S6.
- Armstrong AW, Mehta MD, Schupp CW, Gondo GC, Bell SJ, Griffiths CEM. Psoriasis in in the United States. JAMA Dermatol. 2021;157(8):1-7. doi:10.1001/jamadermatol.2021.2007
- Transparency Market Research. Psoriasis to $121 by 2024. Pharmaceutical Processing World. June 14, 2019. Accessed December 4, 2023. https://www.pharmaceuticalprocessingworld.com/psoriasis-treatment-market-to-gain-121-billion-by-2024/
- Gordon KB, Foley P, Krueger JG, et al. Bimekizumab efficacy and safety in moderate to severe plaque psoriasis (BE READY): a multicentre, double-blind, placebo-controlled, randomised withdrawal phase 3 trial. Lancet. 2021;397(10273):475-486. doi:10.1016/S0140-6736(21)00126-4
- McInnes IB, Asahina A, Coates LC, et al. Bimekizumab in patients with psoriatic arthritis, naive to biologic treatment: a randomised, double-blind, placebo-controlled, phase 3 trial (BE OPTIMAL). Lancet. 2023;401(10370):25-37. doi:10.1016/S0140-6736(22)02302-9
- Jin W, Dong C. IL-17 cytokines in immunity and inflammation. Emerg Microbes Infect. 2013;2(9):e60. doi:10.1038/emi.2013.58
- Goodrich D. A review of newly available Humira biosimilars for pharmacists. November 22, 2023. Accessed December 6, 2023. https://www.pharmacypracticenews.com/Review-Articles/Article/12-23/A-Review-of-Newly-Available-Humira-Biosimilars-for-Pharmacists/72110?ses=ogst
- Biosimilars. FDA. March 3, 2023. Accessed December 6, 2023. https://www.fda.gov/drugs/therapeutic-biologics-applications-bla/biosimilars
- Menter A, Cohen S, Kay J, et al. Switching between adalimumab reference product and BI 695501 in patients with chronic plaque psoriasis (VOLTAIRE-X): a randomized controlled trial. Am J Clin Dermatol. 2022;23(5):719-728. doi:10.1007/s40257-022-00708-w
- García-Beloso N, Altabás-González I, Samartín-Ucha M, et al. Switching between reference adalimumab and biosimilars in chronic immune-mediated inflammatory diseases: systematic literature review. Br J Clin Pharmacol. 2022;88(4):1529-1550. doi:10.1111/bcp.15101
- Wehrwein P. 8 Humira biosimilars are on the market. Managed Healthcare Executive. July 4, 2023. Accessed December 6, 2023. https://www.managedhealthcareexecutive.com/view/8-humira-bosimilars-are-on-the-market
- Milakovic M, Gooderham MJ. Phosphodiesterase-4 inhibition in psoriasis. Psoriasis (Auckl). 2021;11:21-29. doi:10.2147/PTT.S303634
- Lebwohl MG, Kircik LH, Moore AY, et al. Effect of roflumilast cream vs vehicle cream on chronic plaque psoriasis: the DERMIS-1 and DERMIS-2 randomized clinical trials. JAMA. 2022;328(11):1073-1084. doi:10.1001/jama.2022.15632
- Kircik LH, Alonso-Llamazares J, Bhatia N, et al. Once-daily roflumilast foam 0.3% for scalp and body psoriasis: a randomized, double-blind, vehicle-controlled phase IIb study. Br J Dermatol. 2023;189(4):392-399. doi:10.1093/bjd/ljad182
- Zirwas MJ, Draelos ZD, DuBois J, et al. Efficacy of roflumilast foam, 0.3%, in patients with seborrheic dermatitis: a double-blind, vehicle-controlled phase 2a randomized clinical trial. JAMA Dermatol. 2023;159(6):613-620. doi:10.1001/jamadermatol.2023.0846
- Fiorillo L, Becker E, de Lucas R, et al. Efficacy and safety results of apremilast in pediatric patients with moderate to severe plaque psoriasis: 16-week results from SPROUT, a phase 3, randomized, controlled study. SKIN J Cutan Med. 2023;7(2):s109. doi:10.25251/skin.7.supp.109
- Positive new data from Otezla studies, SPROUT, for pediatric plaque psoriasis and DISCREET for genital psoriasis. September 9, 2022. Accessed December 8, 2023. https://www.medthority.com/news/2022/9/positive-new-data-from-otezla-studies-sprout-for-pediatric-plaque-psoriasis-and-discreet-for-genital-psoriasis.—amgeb/
- Smith T. FDA grants approval of roflumilast cream 0.3% for psoriasis patients aged 6 to 11. HCP Live. October 6, 2023. Accessed December 9, 2023. https://www.hcplive.com/view/fda-grants-approval-roflumilast-cream-for-psoriasis-patients-aged-6-to-11
- Andrus E. Important and upcoming developments in psoriasis. Dermatology Times. April 13, 2023. Accessed December 8, 2023. https://www.dermatologytimes.com/view/important-and-upcoming-developments-in-psoriasis
- Brunk D. What does the future of psoriasis treatment look like? MDedge. February 21, 2023. Accessed December 8, 2023. https://www.mdedge.com/dermatology/article/261330/psoriasis/what-does-future-psoriasis-treatment-look
- Dhalla AK, Al-Shamsie Z, Beraki S, et al. A robotic pill for oral delivery of biotherapeutics: safety, tolerability, and performance in healthy subjects. Drug Deliv Transl Res. 2022;12(1):294-305. doi:10.1007/s13346-021-00938-1