- General Dermatology
- Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Anti-Aging
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
Image IQ: A 43-year-old man with a symmetrical palpable purpura rash on his legs
Image IQ: A 43-year-old man with a symmetrical palpable purpura rash on his legs. What’s your diagnosis?
Image IQ: A 43-year-old man with a symmetrical palpable purpura rash on his legs. What’s your diagnosis? (Photo courtesy of VisualDx 2018)
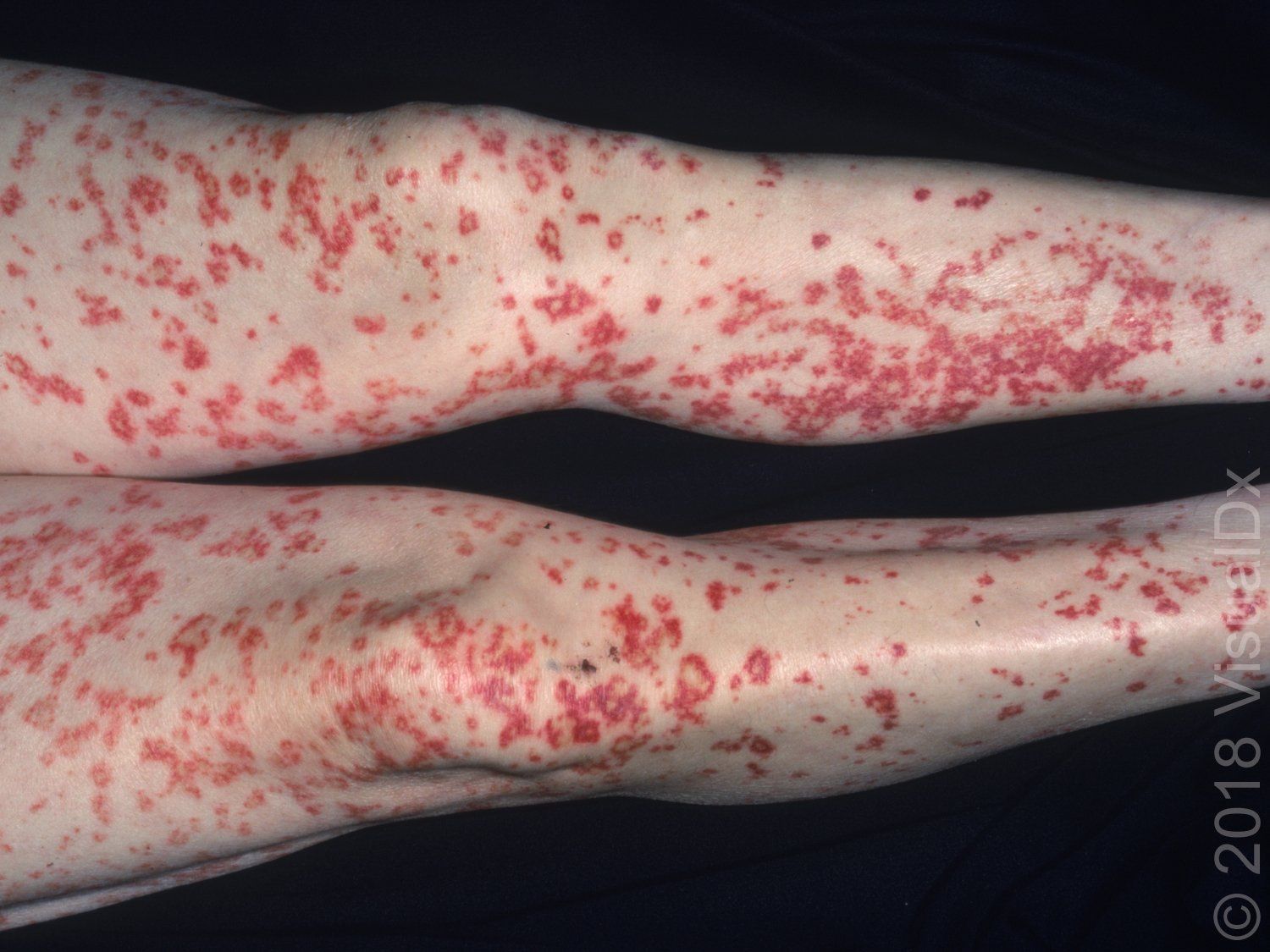
A 43-year-old man was treated in the emergency department with a symmetrical rash of palpable purpura on his legs. He complained of a fever and arthralgia, but no headache or neck pain. The patient disclosed a current infection with hepatitis C virus.
What’s your diagnosis?
A. Rocky Mountain spotted fever
B. Leukocytoclastic vasculitis
C. Sjogren syndrome
D. Acute meningococcemia
Click on the next page for the answer.
The correct answer is B: Leukocytoclastic vasculitis
Leukocytoclastic vasculitis (LCV) is a small vessel vasculitis that predominantly affects postcapillary venules in the dermis.
LCV can occur in all ages and in both sexes. It is more commonly found in adults, but up to 10% of cases are in the pediatric population. The clinical hallmark of LCV is palpable purpura: purpuric papules erupt symmetrically on the shins 7-10 days after an inciting factor. Other parts of the lower extremities may be involved including thighs and dorsal feet. Less frequently, the buttocks, upper extremities, and abdomen are involved. Initially, purpuric macules may be seen that give way to palpable purpura. In more advanced cases, bullae and ulcers may be seen. While the majority of cases are asymptomatic, LCV can be associated with pruritus, pain, or burning.
A variety of inciting factors have been identified, including medications (especially antibiotics, NSAIDs, and diuretics), pathogens (hepatitis viruses, human immunodeficiency virus [HIV], Epstein-Barr virus, and streptococci), malignancy, inflammatory bowel disease, or connective tissue disease (systemic lupus erythematosus [SLE], Sjögren syndrome, and rheumatoid arthritis). Up to 50% of cases, however, have no identifiable cause and are considered idiopathic.
Pathogenically, antigen-antibody complexes bind to the endothelium. The complement cascade is subsequently activated, effecting neutrophil chemotaxis. Vessel wall damage then ensues secondary to proteolytic enzymes and reactive oxygen species released by neutrophils.
The physician will need to differentiate skin-limited LCV from systemic vasculitis and should suspect the latter if fever, myalgias, malaise, lymphadenopathy, abdominal pain, melena, hematochezia, diarrhea, hematuria, lower extremity swelling, or paresthesias are noted. The level of systemic involvement will largely influence the prognosis. Over 90% of patients with LCV limited to the skin will experience spontaneous resolution over several weeks to months.
ICD 10 Code: L95.8 – Other vasculitis limited to the skin
For more information about this quiz â specifically, differential diagnoses and pitfalls, clinical tests, management pearls, therapy and a complete list of references â visit VisualDx online.
